Infantile pyloric stenosis
| Normal anatomy |
|
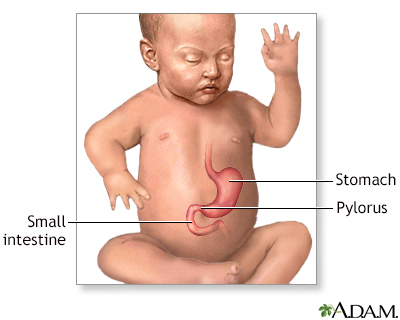
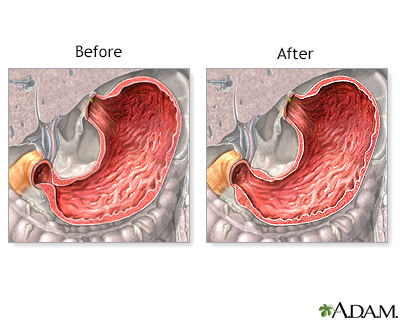
The stomach connects the esophagus to the small intestines The pylorus of the stomach is a small, narrow muscular sphincter through which food passes into the duodenum after it has been partially digested in the stomach.
|
|
| Indications |
|
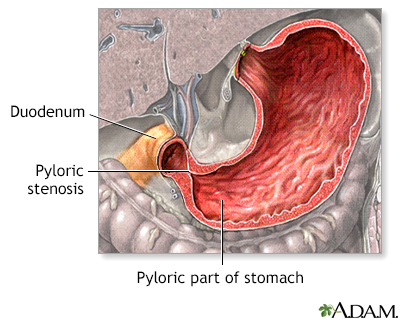
Pyloric stenosis is a congenital defect in which the opening of the pylorus is too narrow. Food is thus unable to pass into the duodenum. Children with pyloric stenosis usually manifest forceful, "projectile" vomiting within the first 1 to 2 weeks of life.
|
|
| Incision |
|
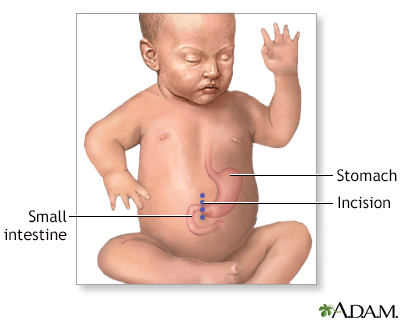
After general anesthesia is administered and the patient is in deep sleep and pain free, the abdomen is cleaned and draped. A small incision is made in the abdomen.
|
|
| Procedure |
|
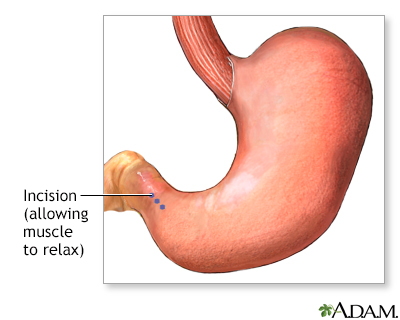
The surgeon makes a cut into the pyloric muscle (stomach outlet) down to the mucosa, the inner layer of the stomach, thus releasing the restriction. No tissue is removed and the stomach lining is not opened. The pyloric muscle returns to normal size with time.
|
|
| Aftercare |
|
Children usually recover quickly. There are no long-term disadvantages to surgery. One to two days of hospitalization may be all that is required. Feedings by mouth are usually delayed for 12 hours after the operation. The stomach requires this short time to regain its ability to contract and to empty. Most infants can advance from clear liquids to normal amounts of formula or breast feedings within 36 hours after the operation. Vomiting of one or two feedings in the first 24 to 48 hours after the operation is not uncommon. Paper tapes will cover a small incision located on the child's right upper abdomen. A firm ridge may appear at the incision site, which is no cause for concern. Avoid bathing for at least 5 days after the operation. Sponge bathing is permitted the day of discharge. Carefully pat dry the incision tapes after the sponge bath.
|
|

|
Review Date:
8/5/2023
Reviewed By:
Neil K. Kaneshiro, MD, MHA, Clinical Professor of Pediatrics, University of Washington School of Medicine, Seattle, WA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team. |
The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed medical professional should be consulted for diagnosis and treatment of any and all medical conditions. Links to other sites are provided for information only -- they do not constitute endorsements of those other sites. No warranty of any kind, either expressed or implied, is made as to the accuracy, reliability, timeliness, or correctness of any translations made by a third-party service of the information provided herein into any other language. © 1997-
A.D.A.M., a business unit of Ebix, Inc. Any duplication or distribution of the information contained herein is strictly prohibited.
© 1997-

All rights reserved.