Tracheostomy
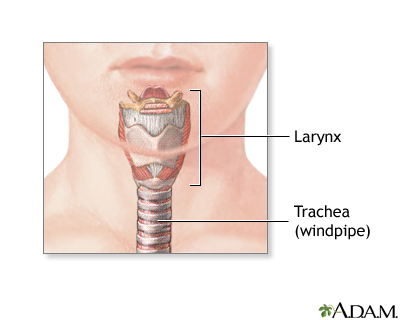
| Normal anatomy |
|
The trachea, or windpipe, carries air from the larynx to the bronchi and lungs.
|
|
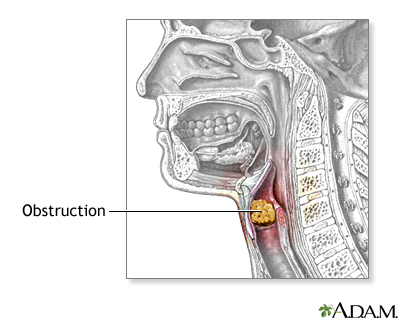
| Indications |
|
The indications for tracheostomy include:
- Prolonged intubation during the course of a critical illness
- Subglottic stenosis from prior trauma
- Obstruction from obesity for sleep apnea
- Congenital (inherited) abnormality of the larynx or trachea
- Severe neck or mouth injuries
- Inhalation of corrosive material smoke or steam
- Presence of a large foreign body that occludes the airway
- Paralysis of the muscles that affect swallowing causing a danger of aspiration
- Long term unconsciousness or coma
|
|
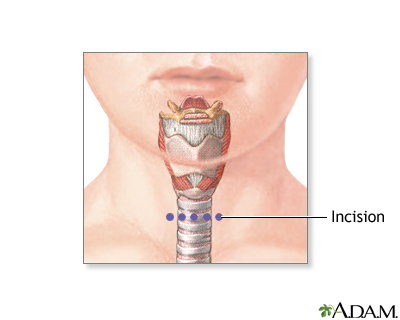
| Incision |
|
General anesthesia is used and the patient is deep asleep and pain-free. The neck is cleaned and draped. Incisions are made to expose the tough cartilage rings that make up the outer wall of the trachea.
|
|
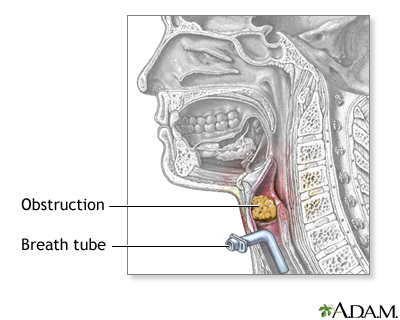
| Procedure |
|
The surgeon then cuts two of these rings and inserts a tracheostomy tube.
|
|
| Aftercare |
|
Most patients require 1 to 3 days to adapt to breathing through a tracheostomy tube. Communication will require adjustment. Initially, it may be impossible for the patient to talk or make sounds. After training and practice, most patients can learn to talk with a trach tube.
Patients or parents learn how to take care of the tracheostomy during the hospital stay. Home-care service may also be available. Normal lifestyles are encouraged and most activities can be resumed. When outside a loose covering for the tracheostomy stoma (hole) (a scarf or other protection) is recommended. Other safety precautions regarding exposure to water, aerosols, powder or food particles must be adhered to.
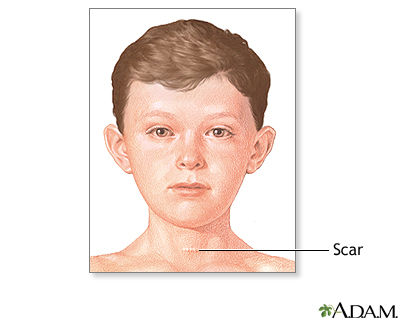
After treatment of the underlying problem that necessitated the tracheostomy tube initially, the tube is easily removed, and the hole heals quickly, with only a small scar.
|
|

|
Review Date:
1/1/2025
Reviewed By:
Frank D. Brodkey, MD, FCCM, Associate Professor, Section of Pulmonary and Critical Care Medicine, University of Wisconsin School of Medicine and Public Health, Madison, WI. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team. |
The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed medical professional should be consulted for diagnosis and treatment of any and all medical conditions. Links to other sites are provided for information only -- they do not constitute endorsements of those other sites. No warranty of any kind, either expressed or implied, is made as to the accuracy, reliability, timeliness, or correctness of any translations made by a third-party service of the information provided herein into any other language. © 1997-
A.D.A.M., a business unit of Ebix, Inc. Any duplication or distribution of the information contained herein is strictly prohibited.
© 1997-

All rights reserved.