| Mold allergy |
Along with pollens from trees, grasses, and weeds, molds are an important cause of seasonal allergic rhinitis. People allergic to molds may have seasonal allergic rhinitis symptoms from spring to late fall due to outdoor mold exposure. The mold season often peaks from July to late summer. Unlike pollens, molds may persist after the first killing frost. Some can grow at subfreezing temperatures, but most become dormant. Snow cover lowers the outdoor mold count dramatically but does not kill molds. After the spring thaw, molds thrive on the vegetation that has been killed by the winter cold.
In the warmest areas of the United States, however, molds thrive all year and can cause year-round (perennial) allergic problems. Mold can also cause allergic rhinitis symptoms year-round if there is mold indoors (such as mold from water damage or humid rooms) like in a finished basement. Molds growing indoors can cause perennial allergic rhinitis even in the coldest climates.
What is mold?
There are thousands of types of molds and yeast, the two groups of plants in the fungus family. Yeasts are single cells that divide to form clusters. Molds consist of many cells that grow as branching threads called hyphae. Although both groups can probably cause allergic reactions, only a small number of molds are widely recognized offenders.
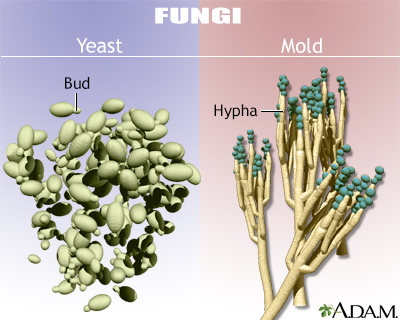
The seeds or reproductive particles of fungi are called spores. They differ in size, shape, and color among species. Each spore that germinates can give rise to new mold growth, which in turn can produce millions of spores.
What is mold allergy?
When inhaled, microscopic fungal spores or, sometimes, fragments of fungi may cause allergic rhinitis. Because they are so small, mold spores may evade the protective mechanisms of the nose and upper respiratory tract to reach the lungs.
In a small number of people, symptoms of mold allergy may be brought on or worsened by eating certain foods, such as cheeses, processed with fungi. Occasionally, mushrooms, dried fruits, and foods containing yeast, soy sauce, or vinegar will produce allergic symptoms.
Where do molds grow?
Molds can be found wherever there is moisture, oxygen, and a source of the few other chemicals they need. In the fall they grow on rotting logs and fallen leaves, especially in moist, shady areas. In gardens, they can be found in compost piles and on certain grasses and weeds. Some molds attach to grains such as wheat, oats, barley, and corn, making farms, grain bins, and silos likely places to find mold.
Hot spots of mold growth in the home include damp basements and closets, bathrooms (especially shower stalls), places where fresh food is stored, refrigerator drip trays, house plants, air conditioners, humidifiers, garbage pails, mattresses, upholstered furniture, and old foam rubber pillows.
Bakeries, breweries, barns, dairies, and greenhouses are favorite places for molds to grow. Loggers, mill workers, carpenters, furniture repairers, and upholsterers often work in moldy environments.
Which molds are allergenic?
Like pollens, mold spores are important airborne allergens only if they are abundant, easily carried by air currents, and allergenic in their chemical makeup. Found almost everywhere, mold spores in some areas are so numerous they often outnumber the pollens in the air. Fortunately, however, only a few dozen different types are significant allergens.
In general, Alternaria and Cladosporium (Hormodendrum) are the molds most commonly found both indoors and outdoors throughout the United States. Aspergillus, Penicillium, Helminthosporium, Epicoccum, Fusarium, Mucor, Rhizopus, and Aureobasidium (Pullularia) are also common.
There is no relationship, however, between a respiratory allergy to the mold Penicillium and an allergy to the drug penicillin, which is made from mold.
Are mold counts helpful?
Similar to pollen counts, mold counts may suggest the types and relative quantities of fungi present at a certain time and place. For several reasons, however, these counts probably cannot be used as a constant guide for daily activities.
One reason is that the number and types of spores actually present in the mold count may have changed considerably in 24 hours because weather and spore dispersal are directly related. Many of the common allergenic molds are of the dry spore type -- they release their spores during dry, windy weather. Other fungi need high humidity, fog, or dew to release their spores. Although rain washes many larger spores out of the air, it also causes some smaller spores to be shot into the air.
In addition to the effect of day-to-day weather changes on mold counts, spore populations may also differ between day and night. Day favors dispersal by dry spore types and night favors wet spore types.
Are there other mold-related disorders?
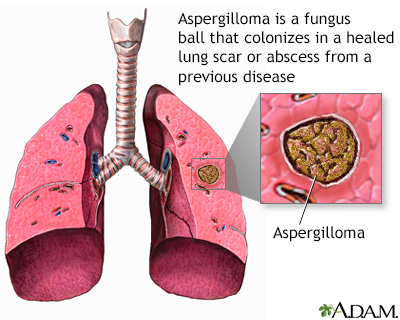
Fungi or organisms related to them may cause other health problems similar to allergic diseases. Some kinds of Aspergillus may cause several different illnesses, including both infections and allergy. These fungi may lodge in the airways or a distant part of the lung and grow until they form a compact sphere known as a "fungus ball." This occurs only in people who have had significant lung problems in the past. In people with other serious underlying illnesses, Aspergillus may grasp the opportunity to invade the lungs or the whole body.
In some individuals, exposure to these fungi also can lead to asthma or to a lung disease resembling severe inflammatory asthma called allergic bronchopulmonary aspergillosis. This latter condition, which occurs only in a minority of people with asthma, is characterized by wheezing, low-grade fever, and coughing up of brown-flecked masses or mucus plugs. Skin testing, blood tests, x-rays, and examination of the sputum for fungi can help establish the diagnosis. Corticosteroid drugs are usually effective in treating this reaction. Immunotherapy (allergy shots) is not helpful.
 |
|
Created by the National Institutes of Health. Illustrations copyright A.D.A.M., Inc.
Reviewed By: Paula J. Busse, MD, Assistant Professor of Medicine, Division of Clinical Immunology, Mount Sinai School of Medicine, New York, NY, Review provided by VeriMed Healthcare Network. Also reviewed by David Zieve, MD, MHA, Medical Director, A.D.A.M., Inc.
